Introduction
Physiotherapy in Bathurst for Foot Issues
Welcome to Physio Max’s guide to Congenital Flatfoot (Pes Planus) in Children.
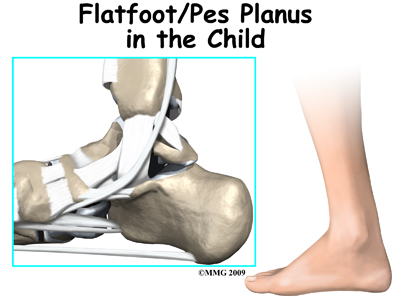
Flatfeet (also known as pes planus) describes a condition in which the longitudinal (lengthwise) and/or medial (crosswise) arches of the foot are dropped down or flat. The entire bottom of the bare foot is in contact with the floor or ground surface during standing, walking, and other weight bearing activities. Congenital means that the condition is present at birth in one or both feet. When only one foot is affected, the problem is referred to as unilateral pes planus or flatfoot. When both feet are involved, the condition is bilateral flatfeet. Sometimes the term ‘fallen arch’ is used, but doctors prefer not to use this term in favor of the more accurate medical term ‘pes planus.’
This guide will help you understand:
- what parts of the foot are affected
- how the problem develops
- how health care professionals diagnose the condition
- what treatment options are available
- what Physio Max’s approach to treatment is
#testimonialslist|kind:all|display:slider|orderby:type|filter_utags_names:Foot therapy|limit:15|heading:Hear from some of our *Foot Therapy* patients#
Anatomy
What parts of the foot are involved?
The anatomy of the foot is very complex. When everything works together, the foot functions correctly. When one part becomes damaged, it can affect every other part of the foot and lead to problems. With a flatfoot deformity, bones, ligaments, and muscles of the foot are all affected. Areas up the biomechanical chain such as the ankle, the shin, the knee, the hip and the low back can also be affected due to the misalignment that occurs.
Related Document: Physio Max's Guide to Foot Anatomy
Bones
The skeleton of the foot centers around the talus, or ankle bone, that forms the main part of the ankle joint. The two bones of the lower leg, the large tibia and the smaller fibula, come together at the ankle joint around the talus to form a very stable structure.
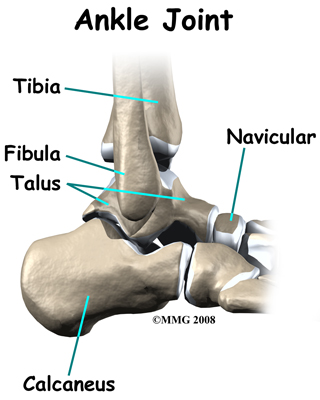 The foot is able to bend up and down due to the joint formed by the tibia, fibula, and talus.
The foot is able to bend up and down due to the joint formed by the tibia, fibula, and talus.
The two bones that make up the back part of the foot (sometimes referred to as the hindfoot) are the talus and the calcaneus. The calcaneus is the heel bone. The talus is connected to the calcaneus at the subtalar joint. The subtalar joint allows the foot to rock from side to side. People with flatfeet usually have more motion at the subtalar joint than people who do not have flatfeet. This increased flexibility of the subtalar joint results in many compensatory actions of the foot and ankle in order to maintain proper foot alignment during standing and walking.
Just down the foot from the ankle is a set of five bones called tarsal bones that work together as a group and are termed the midfoot. These tarsal bones are unique in the way they fit together. There are multiple joints between the tarsal bones. When the muscles of the foot and leg twist the foot inwards, these bones lock together and form a very rigid structure. When they are twisted in the opposite direction, they become unlocked and allow the foot to conform to whatever surface the foot is contacting.
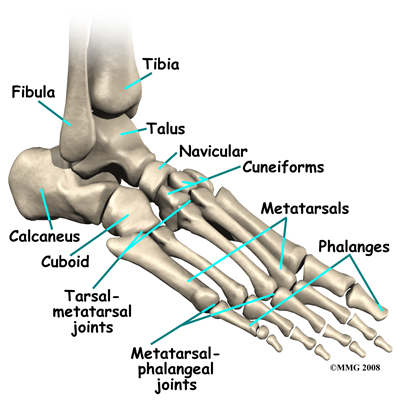
The tarsal bones are connected to the five long bones of the foot called the metatarsals. The two groups of bones are fairly rigidly connected, without much movement at the joints that connect them. Finally, there are the bones of the toes, called the phalanges. The metatarsals and phalanges make up the forefoot.
Ligaments and Tendons
Ligaments are the soft tissues that attach bones to bones. Ligaments are very similar to tendons in their make up however tendons attach muscles to bones rather than bones to other bones. Both of these structures are made up of small fibers of a material called collagen. The collagen fibers are bundled together to form a rope-like structure.
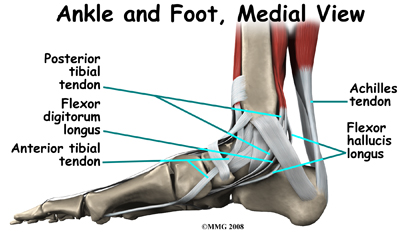
The large Achilles' tendon, at the back of the ankle is the most important tendon for walking, running, and jumping. It attaches the calf muscles to the heel bone to allow us to rise up on our toes. The posterior tibial tendon attaches one of the smaller muscles of the calf to the underside of the foot. This tendon helps support the arch and allows us to turn the foot inward. Failure of the posterior tibial tendon is a major problem in many cases of pes planus.
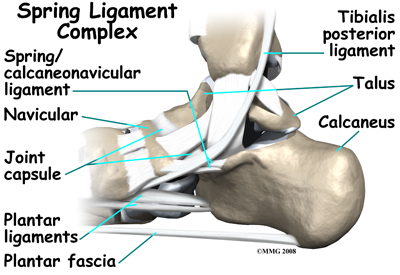
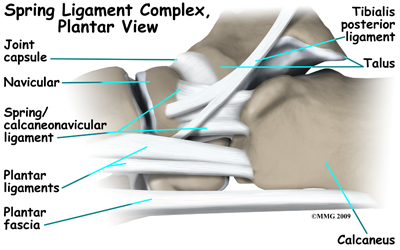
Many small ligaments hold the bones of the foot together. Most of these ligaments form part of the joint capsule around each of the joints of the foot. A joint capsule is a watertight sac that forms around all of the joints of the foot. The capsule is made up of the ligaments around the joint and the soft tissues between the ligaments that fill in the gaps and form the sac.
The plantar fascia is a thick band of ligamentous tissue on the bottom of the foot that extends from the heel to the toes. When you pull your toes back with one hand, you will be able to feel this band with your fingers of the other hand. This fascia is also critical in supporting the long arch of the foot and in creating the rigid foot structure mentioned above.
The spring ligament complex, which supports the talonavicular joint, is often involved in the flatfoot condition. The spring ligament complex works with the posterior tibial tendon and the plantar fascia to support and stabilize the longitudinal arch of the foot. Laxity of the ligaments that support this arch can result in deformity of the foot and/or ankle resulting in pes planus.
Muscles
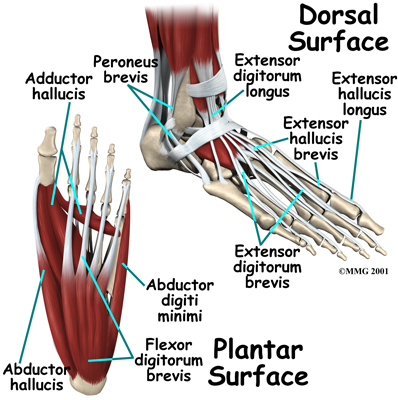 The strong muscles and tendons in the lower leg that connect directly to the foot create most of the motion of the foot. Contraction of these muscles is the main way that we move our feet to stand, walk, run, and jump.
The strong muscles and tendons in the lower leg that connect directly to the foot create most of the motion of the foot. Contraction of these muscles is the main way that we move our feet to stand, walk, run, and jump.
There are numerous small muscles in the foot. While these muscles are not nearly as important as the similar small muscles in the hand, they do affect the way that the toes work. Most of the muscles of the foot are arranged in layers on the sole of the foot (the plantar surface). There they connect to and move the toes as well as provide padding underneath the sole of the foot. Damage to these muscles can cause problems in the foot.
Causes
What causes this problem?
 Most babies and young children have what looks like flat feet but this is normal for them. In a baby much of the foot and ankle are still made up of soft tissue, fat, and cartilage and the arch has not formed fully yet. Eventually as the baby gets older the cartilage calcifies into the normal bones of the foot. When the child starts to get up on their feet to begin walking the joints are still hypermobile. This is when the flatfoot deformity becomes obvious and parents may become concerned that something is wrong with their child's foot. The vast majority of children will grow out of the flat foot within their first decade of life. Stress and activities during early childhood requiring strength in the feet are actually the training needed to develop normal muscle, tendon, ligaments, and bone in the foot and ankle. In some cases, unfortunately, the arch doesn't form and the foot remains flat into late childhood, adolescence, and adulthood.
Most babies and young children have what looks like flat feet but this is normal for them. In a baby much of the foot and ankle are still made up of soft tissue, fat, and cartilage and the arch has not formed fully yet. Eventually as the baby gets older the cartilage calcifies into the normal bones of the foot. When the child starts to get up on their feet to begin walking the joints are still hypermobile. This is when the flatfoot deformity becomes obvious and parents may become concerned that something is wrong with their child's foot. The vast majority of children will grow out of the flat foot within their first decade of life. Stress and activities during early childhood requiring strength in the feet are actually the training needed to develop normal muscle, tendon, ligaments, and bone in the foot and ankle. In some cases, unfortunately, the arch doesn't form and the foot remains flat into late childhood, adolescence, and adulthood.
Even if the deformity does not fully correct with age, it does not always cause direct problems with the foot, although the altered biomechanics due to the flatfoot can still affect the alignment of the lower extremity chain. The shin, knee, hip and back are all affected by the position of the foot, so if pain in any of these areas crops up later in life, the flat foot will be noted as a contributing factor and will need to be addressed at that point. It should be noted that flatfeet can be an inherited condition so looking at the feet of the parents may give an indication as to whether or not the flatfeet will correct as the child ages.
There is no one specific cause of flatfoot deformity that can be identified. There are many possible biomechanical causes that can create the condition. Many soft tissue structures such as the ligaments and muscles in the foot must connect and support one another to form the proper arch and prevent a flatfoot deformity. Tibial (lower leg bone) rotation, hindfoot alignment, and position of the joints of the foot, midfoot, hindfoot, and ankle are all important factors.
Flexible flatfoot refers to a foot that looks flat when standing but appears to have an arch when the foot isn't resting on the floor or against a flat surface. In the flexible flatfoot, the bone alignment is usually normal but the supporting ligaments are lax or loose which creates joints that are hypermobile (move too much). As the soft tissues and joints of the foot and ankle try to maintain a normal foot position, increased stress is placed on them. This can lead to fatigue and loss of strength resulting in a sagging of the arch. This then affects the chain of anatomical structures all the way up the leg.
There are some uncommon causes of flatfoot that result from a congenital defect in the bones. A tarsal coalition refers to a condition where two or more bones in the midfoot or hindfoot fail to form separately during development. The bones remain connected together, which alters the bone structure of the foot and limits the foot’s flexibility. In fact, the foot is quite rigid rather than flexible due to the abnormal connection between the bones of the foot. If the muscles on the outside of the foot are increased in their tone, it can lead to what is called a peroneal spastic flatfoot. This condition is often linked to tarsal coalition, but other conditions such as congenital arthritic or neurological conditions can also be the cause. Some children are born with an extra bone on the inside of their foot, called an accessory navicular. Having this extra bone itself does not necessarily cause a problem but it can create biomechanical changes in how the child uses the foot if the bone is excessively large, or the ligaments supporting it get injured.
Symptoms
What does the condition feel like?
For most young children, the flexible flatfoot deformity is mild and causes no symptoms. They do not suffer from pain, swelling, or sore feet. Children with flexible flatfoot deformity may wear out shoes a bit differently from a normal person, but this is not usually any reason to be concerned.
In moderate to severe cases, the child may report fatigue and tired, sore feet after standing on them all day. During those times, they may limit their own activities to avoid the pain.
In some severe cases, calluses may appear along the longitudinal arch area where pressure occurs as the bones make contact with the floor or hard surface. Excess pressure on the surrounding soft tissues (ligaments, capsules, tendons, muscles) from the flatfoot deformity can lead to other problems over time such as hallux valgus (bunions), or problems further up the biomechanical chain such as misalignment of the patella (kneecap), and rotation of the knee and hip also leading to pain in these areas.
When the flatfoot deformity is the result of a tarsal coalition, the situation may present quite differently. The foot may become painful early on. The child may begin to complain of foot and ankle pain after a minor twisting injury and the pain may not resolve after a normal healing period. The symptom of pain combined with the flatfoot deformity and decreased foot motion should be enough to indicate the more serious problem of tarsal coalition.
Diagnosis
How do health care professionals diagnose the problem?
The history and physical examination are probably the most important tools that health care professionals, including your physiotherapist at Physio Max, will use to diagnose this problem. The wear pattern on your child’s shoes can offer some helpful clues as it may show wear and tear on the medial sole rather than the lateral posterior sole, which would be normal. The alignment of your child’s hips, knees, ankles and feet will be observed in both standing and sitting. Your child may be asked to twist their body with their feet planted on the ground, squat, walk, or jump without shoes so their therapist can observe their feet and arches as they move.
A very simple test called the wet footprint may be done to look at the foot position. You can even do this test at home. The patient places their foot in water and then places the foot down on a piece of paper or thin cardboard. After making a footprint, the foot is lifted off the paper. Someone with a flat foot will leave a complete footprint where the sole makes contact with the paper rather than just the print of the toes and lateral foot that would be seen in someone with a normal arch.
Next your therapist will assess the position and mobility of the bones in your child’s forefoot, midfoot, hindfoot, and ankle to determine if there is any subluxation, laxity, or stiffness. This will help to differentiate a flexible flatfoot from rigid flatfoot.
The strength of the muscles in the foot and lower leg will also be assessed. Muscle testing helps identify any areas of weakness or muscle imbalance. This will be done in both the weight bearing and non-weight bearing positions. An important test that can help identify insufficient posterior tibial tendon problems is the single heel raise. Your therapist will ask your child to stand on one foot and rise up on their toes. They should be able to lift their heel off the ground easily while keeping the heel bone (calcaneus) centered and slightly turned inward (inverted) and their knees straight. If they cannot, their posterior tibialis muscle and tendon may be impaired.
In addition to looking at the muscles close to the foot, your physiotherapist will assess the strength in the muscles of your child’s hip, as these muscles also play a part in controlling the alignment of your lower leg as well as lifting the arch of your foot. The biomechanical link between the hip and foot can be felt if you stand relaxed and squeeze both buttocks muscles together. As you do this you will feel the arches of your feet slightly lift. It is for this reason that control around the foot cannot only be left to the joints and muscles directly connected to the foot. The strong hip muscles will also need addressing if they are shown to be weak or inadequately functioning.
Investigations
X-rays or other more advanced imaging tests such as a CT scan or MRI may be ordered as part of diagnosing pes planus, but these are rarely needed. X-rays will show, however, if there is an accessory navicular or tarsal coalition as part of the problem. In most cases, however, your health care professional may be able to see and feel a prominent bump with tenderness around the medial side of the foot when an accessory navicular bone is present, or if there is a tarsal coalition they may note during the assessment that there is no motion between the foot bones in this area.
Physio Max provides services for physiotherapy in Bathurst.
Treatment
What treatment options are available?
Nonsurgical Treatment
If your child is quite young there may be no treatment needed for mild cases of flatfeet, especially flexible flatfeet. This condition often corrects itself in time as the child grows and develops. These children should be encouraged to walk barefoot whenever it is safe to do so as this will increase sensory input into the foot. At the same time, navigating various floor and ground surfaces helps build strength and stability in the foot.
Older children and adults will benefit from treatment with a physiotherapist at Physio Max. One of the first things your therapist will discuss with you are your child’s shoes. Sometimes a simple modification to the shoe may reduce the fatigue and discomfort in the foot. Even simply purchasing comfortable shoes with a good arch support, firm heel counter (back of the heel), and a flexible sole (bottom) can make a difference. Supporting the arch helps decrease the tension in the posterior tibialis tendon. For other patients, your therapist may suggest an off-the-shelf (prefabricated) shoe insert as they can work well. The goal is to support the foot and prevent further stretching of lax ligaments and tendons. These supports will not reverse the structural deformity and they will not build an arch by wearing them over time. The inserts simply help the shoe better fit the foot and support the structures of the foot to prevent further deformity. Improving alignment can take tension off the soft tissue structures, reduce fatigue, and improve the biomechanics of standing and gait (walking). Your therapist may recommend that you purchase custom made orthotics for your child. Custom fit orthotics are recommended for any individual who has a significant arch drop, or for whom prefabricated inserts do not relieve their symptoms or position their arch adequately. Often taping the bottom of the foot, which your physiotherapist can do, and can teach you to do for your child, can be trialed before expensive orthotics are purchased. Taping may be enough in mild cases of pes planus, as long as your child can learn to control the position of their foot and can maintain this position during high-level activities. In most cases shoe inserts or orthotics, even pre-fabricated ones, will significantly improve any pain related to pes planus, and will be recommended to both relieve symptoms but also to avoid future progression of the injury.
If your child has developed any pain from their flatfoot your physiotherapist can help to relieve their discomfort. They may use ice, heat, ultrasound, or other electrical modalities on the bottom of the foot or along the lower leg to provide relief. Icing or heating the arch at home will provide similar relief. Your therapist may massage the bottom of the foot or calf, which can be particularly useful in relieving the discomfort.
Unfortunately these treatments only provide temporary relief; addressing the real problem of the fallen arch and misalignment, will provide more long-term relief to your child’s injury.
If your child has pain in their feet then they will likely need a modified rest period to help relieve their symptoms. Your physiotherapist will strongly advise avoiding any activities that cause discomfort while your child still has symptoms. This may also mean resting for a short period from any sport they do, or at least decreasing the amount of activity they partake in over a period of time. Your physiotherapist will specifically guide your child regarding the needed rest for their individual injury. This rest may seem quite difficult to achieve, however it is well known that without a relative rest for a painful foot, there is little chance for it to heal. This period of rest where the foot is not being aggravated also greatly improves the ability of the physiotherapy treatment to improve the symptoms. Your physiotherapist will advise your child when it is safe to slowly start back to their activity after this rest period.
Your physiotherapist will prescribe strengthening exercises for your child’s foot and posterior tibialis muscle to help support the fallen arch. As mentioned above, these muscles work to lift the arch of the foot, along with the muscles of the hip, which also help to lift the arch and control alignment down the lower leg chain. An exercise band may be used to provide added resistance to the muscles of the foot, and to strengthen the hip muscles. Your therapist may also prescribe stretching exercises, particularly for the muscles of your calf, which, when tight, can force the hindfoot and then subsequently the mid and forefoot out of alignment.
Being that children are born with pes planus, it is common for patients to not even notice how flat their feet are compared to others. The position of their feet becomes their ‘normal’ position. Re-learning the proper position of the arch is crucial to relieving any pain caused by pes planus as well as to stopping the progression of any deformity. Proprioception is the term used to describe one’s sense of joint position. Your therapist will teach your child what the correct position of their foot and arch should be and will give them exercises that challenge the proprioception of their knee, foot, ankle, and arch. Initially these exercises may be done while they are sitting but as they progress, your physiotherapist will advance the exercises so they are doing them in standing, and eventually just on one foot at a time. The standing position is an important position to work up to as it is much more functional in mimicking normal everyday activities such as walking or stair climbing. Eventually your physiotherapist will prescribe exercises that are extremely challenging, especially if your child is involved in a high-level sport.
Exercises such as squatting and jumping will be added and your child will be required to do these activities while maintaining proper foot and leg alignment, as well as arch control.
It is crucial that your child pays particular attention to the alignment of their arch, foot, ankle, and lower limb as they perform any of the exercises your physiotherapist prescribes. Poor alignment of any of these areas can begin re-creating a situation where they are prone to the flat foot position and can cause pain. Your physiotherapist will repeatedly remind your child to be conscious of the overall alignment of the entire lower limb during both the rehabilitation exercises they do at Physio Max as well during everyday activities such as walking and stair climbing. You, as the parent, will need to be conscious of the correct alignment as well and help to remind your child during their exercises and everyday activities.
Excess body weight will add to the problem of pes planus, so if your child is obese or even moderately overweight, their symptoms and arch drop will be accentuated. Losing excess weight can greatly improve any pain they feel in their foot and decrease the strain on their arch. Your physiotherapist at Physio Max can discuss weight loss strategies and if need be, refer your child to a Nutritionist who can also assist with this goal. Often it is difficult to exercise and increase energy expenditure to lose weight if there is pain associated with the feet, however, there are several safe activity options that your therapist can discuss, such as stationary cycling or swimming.
Physio Max provides services for physiotherapy in Bathurst.
Surgery
Surgery is rarely needed for pes planus. Patients with severe, disabling symptoms that do not respond to conservative care may benefit from further orthopedic evaluation and treatment. In rare cases, surgical intervention to correct the problem and realign the foot may be suggested.
Children with tarsal coalition or an accessory navicular bone require orthopedic evaluation and management. If required, surgery is done to correct the problem by the early teen years (before skeletal maturity). In some cases, more than one operation is needed as the child grows and develops. Pain relief and joint stability are the goals.
Post-surgical Rehabilitation
What should be expected with post-surgical recovery?
Postoperative care will depend on the type of surgery that has been done. There will be a period of immobilization in a cast or removable boot following surgery for a tarsal coalition or an accessory navicular bone. If the surgeon suggests it, a physiotherapist may visit your child in the hospital to start a few simple exercises and to instruct your child on how to walk with crutches. Once your child has been discharged from the hospital physiotherapy at Physio Max can begin as soon as the surgeon indicates it is safe. Generally this is after the period of immobilization is over.
Post-surgical rehabilitation at Physio Max will initially focus on minimizing the pain and swelling from the surgery. The foot will be quite stiff after being immobilized and will feel sore as your child starts to move it. Similar to non-surgical rehabilitation, your physiotherapist may use modalities such as ice, ultrasound, or interferential current to decrease any pain that is lingering. They may also use gentle massage around the muscles of the foot and lower leg. Your physiotherapist will guide your child on when to increase the weight-bearing load on their surgical foot if they are still using crutches. They will likely move from using two crutches down to just one, or a cane or stick, before going without any aid at all and putting full weight through their surgical foot.
As your child’s foot heals from the surgery it is advised to avoid going barefoot when possible until the tissues have sufficiently healed, and the muscles have gained enough strength and motor control to assist in controlling the position of the foot. A shoe with a good arch support and control through the hind, mid and forefoot is best.
One of the first exercises your physiotherapist will prescribe will be some gentle range of motion exercises for the foot and ankle to gradually regain full movement and to help decrease the swelling. These exercises may be as simple as ankle circles and pointing then pulling the toes and foot upward. The exercises should be done within a relatively pain-free motion, however, movement will be encouraged even if it causes a slight bit of discomfort as the movement itself can greatly assist with dispersing any swelling as well as improving the overall level of pain. Elevating the foot as often as possible in these early stages can also assist greatly with removing any swelling from the ankle. It is best to elevate the foot higher than the heart to allow gravity to assist with the fluid drainage. If movement of the foot is too painful or not progressing well, your therapist may suggest that your child does their exercises in either a physiotherapy pool or a tub of warm water where both the warmth and the hydrostatic properties of the water make it easier to move.
A stationary bicycle can be very useful in the initial post-surgical stages to assist with gaining ankle range of motion and decreasing swelling, so, if able, your child will be encouraged to use one. Even if they are unable to fully rotate the pedals, the back and forth motion on the bike is an excellent method of slowly encouraging the ankle to regain its full range of motion.
As soon as your child begins treatment at Physio Max your physiotherapist will immediately prescribe exercises that address the proprioception of their foot, ankle and leg, as well as the alignment of the entire lower limb. Regaining a feel for the new position of the foot and arch is crucial to avoiding a recurrence of the flat foot position and to avoid pain in the foot. Simple strengthening exercises for the bottom of the foot, posterior tibialis muscle, as well as the hip muscles will also begin early on. Again, all exercises should be done within a relatively pain-free range of motion, however, some mild discomfort at the end ranges of motion may be felt as your child begins to strengthen the muscles within their new range of movement.
It is crucial that your child pays particular attention to the alignment of their arch, foot, ankle, and lower limb as they perform any of the exercises your physiotherapist prescribes. Poor alignment of any of these areas can begin re-creating a situation where the foot is prone to the flat foot position and can cause pain. Your physiotherapist will continually cue your child to be conscious of the overall alignment of the entire lower limb during both the rehabilitation exercises they do at Physio Max as well during everyday activities such as walking and stair climbing. You, as the parent, will need to be conscious of the correct alignment as well and help to remind your child during their exercises and everyday activities.
Significant improvement in the foot after surgery occurs gradually over a four-to-six month period of time. During that time, your physiotherapist will progress your child’s exercise program, but the appointments at Physio Max will decrease in frequency.
Some prolonged swelling, stiffness, and discomfort is not uncommon even six to 10 months after foot surgery for flatfeet. Standing on their feet for a long time or walking long distances can also cause foot pain or discomfort for quite some time post-surgically. Eventually these symptoms will disperse.
Returning to regular activities will occur slowly over a period of approximately 6-8 months. If your child is eager early on after surgery to get back to some cardiovascular activity, your physiotherapist can advise them regarding a safe intensity and duration of non-weight bearing cardiovascular activities such as swimming or cycling. They will also advise on when it is safe to return to more aggressive activities for the foot and ankle such as running.
Generally post-surgical rehabilitation for pes planus at Physio Max goes extremely well, however, if your child’s pain lasts longer than it should or their rehabilitation is not progressing as quickly as your physiotherapist feels it should be, your therapist will ask you to follow up with your child’s surgeon to ensure there are no complicating factors impeding their recovery.
Portions of this document copyright MMG, LLC.
Physio Max provides services for physiotherapy in Bathurst.






