Introduction
Physiotherapy in Bathurst for Hand
Welcome to Physio Max's patient resource about Mallet Finger Injuries.
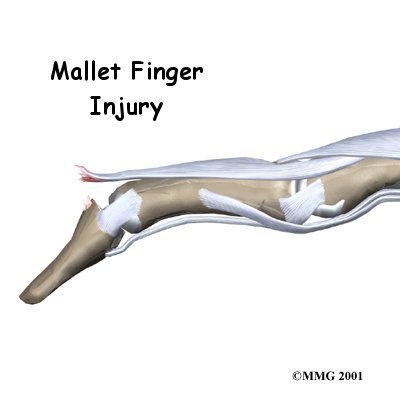
When you think about how much we use our hands, it's not hard to understand why injuries to the fingers are common. Most of these injuries heal without significant problems. One such injury is an injury to the distal interphalangeal, or DIP, joint of the finger. This joint is commonly injured during sporting activities such as baseball. If the tip of the finger is struck with the ball, the tendon that attaches to the small bone underneath can be injured. Untreated, this can cause the end of the finger to fail to straighten completely, a condition called mallet finger.
This article will help you understand:
- what parts make up the DIP finger joint
- what types of injuries affect this joint
- how the injury is treated
- what to expect from treatment
#testimonialslist|kind:all|display:slider|orderby:type|filter_utags_names:Hand Pain|limit:15|heading:Hear from some of our patients who we treated for *Hand Pain*#
Anatomy
What parts of the finger are involved?
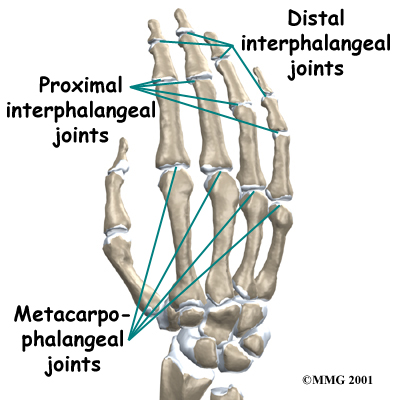
The finger joints work like hinges when the fingers bend and straighten. The main knuckle joint is the metacarpophalangeal joint (MCP joint). It is formed by the connection of the metacarpal bone in the palm of the hand with the first finger bone, or proximal phalanx. Each finger has three phalanges, or small bones, separated by two interphalangeal joints (IP joints). The one closest to the MCP joint (knuckle) is called the proximal IP joint (PIP joint). The joint near the end of the finger is called the distal IP joint (DIP joint).
Finger Joints
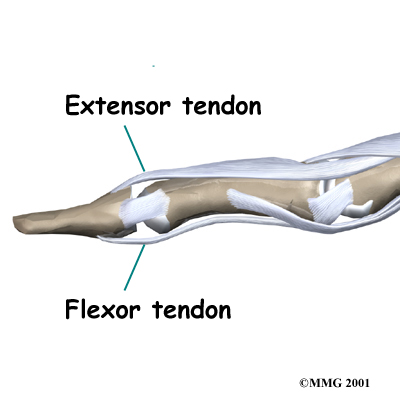
The extensor tendon is attached to the base of the distal phalanx. When it tightens, the DIP joint straightens. Another tendon, the flexor tendon, is attached to the palm of the finger. When it pulls, the DIP joint bends.
Extensor Tendon
Related Document: Physio Max's Guide to Hand Anatomy
Causes
How do these injuries of the DIP joint occur?
A mallet finger results when the extensor tendon is cut or torn from the attachment on the bone. Sometimes, a small fragment of bone may be pulled, or avulsed, from the distal phalanx. The result is the same in both cases: the end of the finger droops down and cannot be straightened.
Symptoms
What do mallet finger injuries look and feel like?
Initially, the finger is painful and swollen around the DIP joint. The end of the finger is bent and cannot be straightened voluntarily. The DIP joint can be straightened easily with help from the other hand. If the DIP joint gets stuck in a bent position and the PIP joint (middle knuckle) extends, the finger may develop a deformity that is shaped like a swan's neck. This is called a swan neck deformity.
Swan Neck Deformity
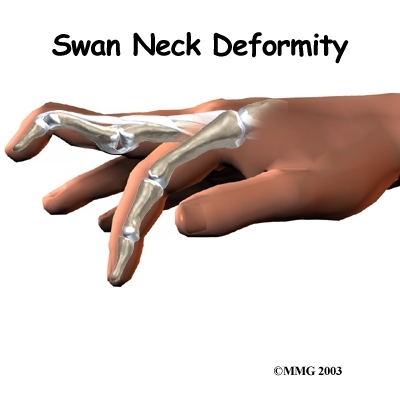
Related Document: Physio Max's Guide to Swan Neck Deformity of the Finger
Diagnosis
What tests will my health care provider do?
When you visit Physio Max, our physiotherapist will take a history and do a physical examination. Usually the diagnosis of mallet finger is clearly evident from the physical exam.

Some patients may be referred to a doctor for further diagnosis. X-rays may be required to see if there is an associated avulsion fracture since this may change the recommended treatment. No other tests are normally required.
Once your diagnostic examination is complete, the physiotherapists at Physio Max have treatment options that will help speed your recovery, so that you can more quickly return to your active lifestyle.
Our Treatment
Non-surgical Rehabilitation
Treatment for mallet finger is usually nonsurgical. If there is no fracture, then the assumption is that the end of the tendon has been ruptured, allowing the end of the finger to droop.
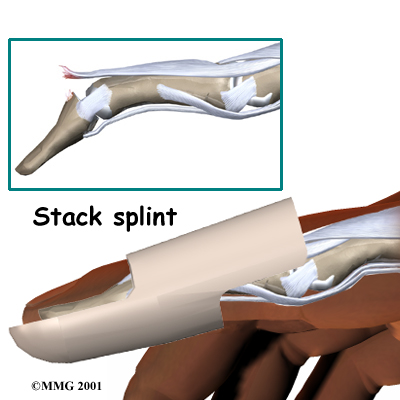
When you begin your physiotherapy program, our physiotherapist may recommend continuous splinting for approximately six weeks followed by six weeks of nighttime splinting.
Usually this will result in satisfactory healing and allow the finger to extend.
The key is continuous splinting for the first six weeks.
The splint holds the DIP joint in full extension and allows the ends of the tendon to move as close together as possible.
As healing occurs, scar formation repairs the tendon.
If the splint is removed and the finger is allowed to bend, the process is disrupted and must start all over again. The splint must remain on at all times, even in the shower.
While a simple homemade splint will work, your physiotherapist can provide you with a 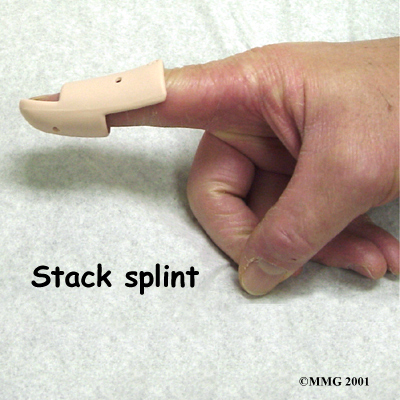 recommendation for the type that will be most beneficial to your recovery. There are many splints that have been designed to make it easier to wear at all times. In some extreme cases where the patient has to use the hands to continue working (such as a surgeon), a metal pin can be placed inside the bone across the DIP joint to act as an internal splint allowing the patient to continue to use the hand. The pin is removed at six weeks.
recommendation for the type that will be most beneficial to your recovery. There are many splints that have been designed to make it easier to wear at all times. In some extreme cases where the patient has to use the hands to continue working (such as a surgeon), a metal pin can be placed inside the bone across the DIP joint to act as an internal splint allowing the patient to continue to use the hand. The pin is removed at six weeks.
Splinting may even work when the injury is quite old. In this case, we will usually splint the finger for about eight to 12 weeks to see if the drooping lessens to a tolerable amount before considering surgery.
When the injury is new, we may recommend that the DIP joint be splinted nonstop in full extension for six to eight weeks. A mallet finger that is up to three months old may require splinting in full extension for eight to 12 weeks. The splint is then worn for shorter periods that include nighttime splinting for six more weeks.
Skin problems are common with prolonged splinting. We advise that you monitor the skin under your splint to avoid skin breakdown. If problems arise, our physiotherapist may recommend new or different splint. Nearby joints may be stiff after keeping the finger splinted for this length of time. Your physiotherapist can design a program of physiotherapy and exercise to assist in finger range of motion and to reduce joint stiffness.
Post-surgical Rehabilitation
Rehabilitation after surgery for mallet finger focuses mainly on keeping the other joints mobile and preventing stiffness from disuse. Our physiotherapy and occupational therapists can teach you home exercises to make sure your other joints do not become stiff. After the surgical pin has been removed, we may gradually introduce exercises to strengthen the finger and increase flexibility.
At Physio Max, our goal is to help speed your recovery so that you can more quickly return to your everyday activities. When your recovery is well under way, regular visits to our office will end. We will continue to be a resource, but you will be in charge of doing your exercises as part of an ongoing home program.
Physio Max provides services for physiotherapy in Bathurst.
Surgery
DIP Fixation
 Surgical treatment is reserved for unique cases.
Surgical treatment is reserved for unique cases.
The first is when the result of nonsurgical treatment is intolerable.
If the finger droops too much, the tip of the finger gets caught as you try to put your hand in a pocket.
This can be quite a nuisance. If this occurs, the tendon can be repaired surgically, or the joint can be fixed in place.
A surgical pin acts like an internal cast to keep the DIP joint from moving so the tendon can heal.
The pin is removed after six to eight weeks.
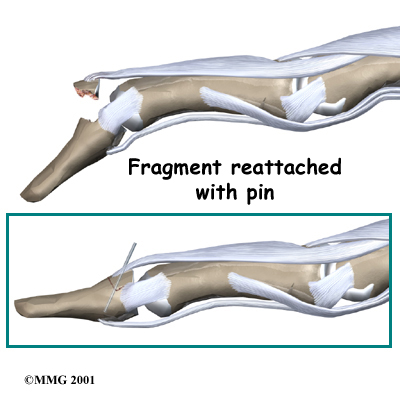
Fracture Pinning
The other case is when there is a fracture associated with the mallet finger.
If the fracture involves enough of the joint, it may need to be repaired.
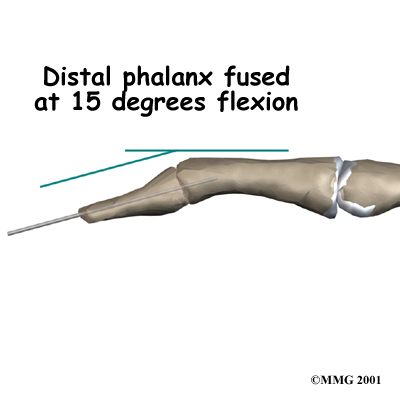
This may require pinning the fracture. If the damage is too severe, it may require fusing the joint in a fixed position.
Pinning the Fracture
Finger Joint Fusion
If the damage cannot be repaired using pin fixation, finger joint fusion may be needed. Joint fusion is a procedure that binds the two joint surfaces of the finger together, keeping them from rubbing on one another. Fusing the two joint surfaces together eases pain, makes the joint stable, and prevents additional joint deformity.
Portions of this document copyright MMG, LLC.